More Topics
◀ Home
What is an explanation of benefits?
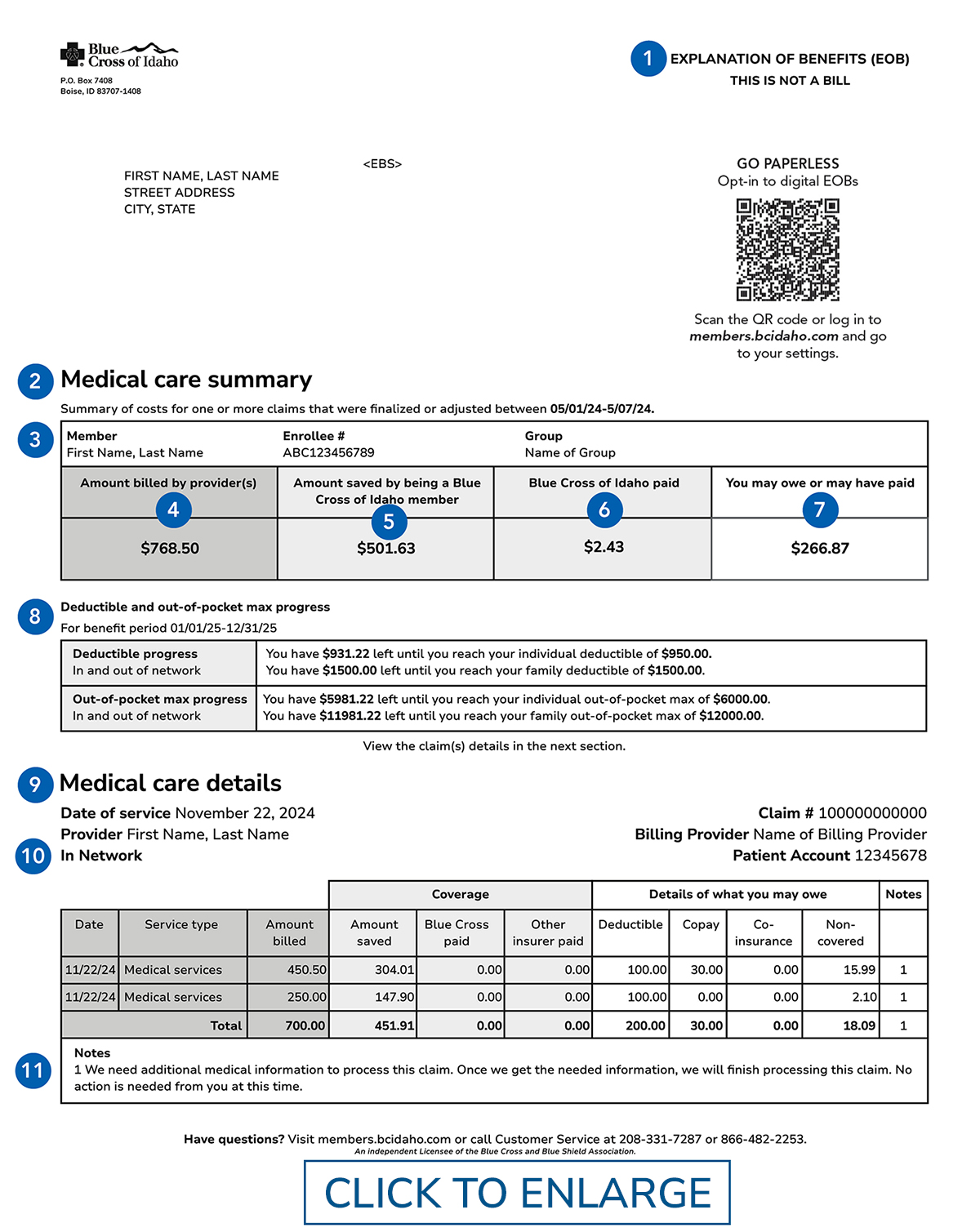
After you get care from a doctor or hospital, you will receive an explanation of benefits (EOB) from Blue Cross of Idaho. An EOB is not a bill – it’s an overview of the care you received, the cost of that care and what we paid for per your plan benefits. You may get a bill from your provider.
 11 key parts of an EOB
11 key parts of an EOB
Even though an EOB isn’t a bill, it’s a good idea to review it and keep it for your records. Here are 11 of the most important parts of the EOB statement:
- THIS IS NOT A BILL
When you get an EOB, keep in mind that it’s not a bill, but an explanation. - Medical care summary
A summary of all charges, coverage, and amount owed for the services referenced in the EOB. - Patient
The person who got the service. This could be you or a family member covered by your plan. - Amount billed by provider(s)
What your provider billed for your care. - Amount saved by being a Blue Cross of Idaho member
The negotiated savings from providers that is passed along to members. - Blue Cross of Idaho paid
This is the amount we paid the provider. - You may owe or have paid
The amount you’re responsible for paying your provider. You should get a bill from the provider’s office that shows the amount you owe and how to pay. - Deductible and out-of-pocket max progress
The amount of your deductible and out-of-pocket maximum you’ve met as of the date of the EOB. - Medical care details
Details of the specific services you received. - Network
Notes whether the provider is or is not part of the Blue Cross of Idaho network. In-network providers agree to charge members less for care. - Notes
Why we processed the claim the way we did.
Get less paper with digital EOBs
Log in to the member website at members.bcidaho.com or visit the Blue Cross of Idaho member app to sign up for digital EOBs and be alerted when a new EOB is ready.
Written by: Blue Cross of Idaho
Posted: June 28, 2021
Updated: January 5, 2026
